
Imagine the following scenario. A patient walks into a hospital with an infectious disease. He sees a physician or a nurse, who diagnoses him, usually on a hunch. In order to try and clear up the infection, the physician prescribes what is essentially a huge cocktail of various antibiotics, in the hope that one of them will solve the problem. Throw stuff at the wall and see what sticks, as they say.
This cocktail either works, and the patient recovers, or it doesn’t, and the patient gets worse or – in many cases – dies. It’s hard to believe, but this is what happens in hospitals all over the developed world at present.
Infectious disease diagnostics and treatment have advanced little in the last 50 years. This has led to the well-documented onset of so called superbugs – infectious diseases that are resistant to currently available antibiotics. MRSA is one. Klebsiella is another. STEC is a third. The list goes on. By 2050, analysts predict antibiotic resistant infectious disease will be responsible for more global deaths than cancer, killing more than 10 million individuals annually. Antibiotic resistance will cause $20 billion excess direct health care costs in the next 35 years, and account for $100 trillion in GDP loss in the US alone. It’s a huge problem, and surprisingly few companies are working to solve it, mostly because the big money is in other diseases.
Merck & Co., Inc. (NYSE:MRK) is one exception. Through its venture capital arm, Merck is funding the development of what looks set to become a big part of the solution to the antibiotic resistance problem. It is one of the main candidates for bringing the space into the 21st century.
By way of its Merck Global Health Innovation Fund, LLC, the company owns a 37.5% stake in the development stage biotech that is driving these advances, OpGen Inc (NASDAQ:OPGN).
The two companies are working together on a combination of projects that could change how we treat, identify and interact with infectious diseases in healthcare facilities and beyond. It sounds like an exaggeration, but here’s where we stand now.
The current method of diagnosis and treatment is an analog process. Any testing takes days, and results are variable. It’s not an efficient way of doing things, especially with life-threatening infections. OpGen has put together a system that is designed to shift the space from analog to digital. It is targeting what the company refers to as the Golden Hour – a one-hour period during which a physician can test, identify and diagnose an infectious disease, but not only that, also treat that infectious disease with the antibiotic most likely to be effective against it rather than a cocktail of hit-or-miss.
The company currently has a diagnostics test in hospitals, commercially available and used globally, called QuickFish. It’s designed to identify which pathogen is involved in the infection in 20 minutes. OpGen is currently trying to get this approved with a digital imager to improve its usability. This is the company’s bread and butter right now, hence its noteworthiness.
Why is it only a legacy tech? Because identifying the pathogen in 20 minutes is a huge advantage over the current system, but it doesn’t complete the picture. Even if physicians know which pathogen to treat, they may now know which antibiotics the pathogen is resistant to. Two versions of the same pathogen can have totally different resistance profiles, and without genetic testing, there’s no way of telling one from the other.
This is where the potentially disruptive technology comes in. OpGen has developed what it calls Acuitas. It’s a one-hour antibiotic resistance test, and it’s designed to work in tandem with a proprietary system called Acuitas Lighthouse. The latter is essentially a giant database that stores information regarding pathogens, antibiotic resistance genes and treatment options.
How it works is first, a patient comes into a hospital, just as above, with an infectious disease. The physician administers the Acuitas test, and within one hour has results that detail the pathogen, and the antibiotic resistance profile of that specific pathogen. The data is then fed into Acuitas Lighthouse, and Lighthouse serves up results similar to those below:
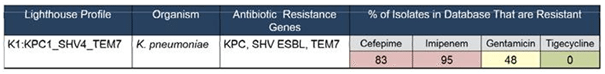
The Lighthouse Profile is basically a reference point in the system. It’s what this particular patient’s pathogen is stored as for current and future use. The organism is that pathogen – in this instance, its K pneumoniae. Currently, it can take 24 hours or more to get just this one bit of information. Within the hour, however, the Acuitas Lighthouse system also returns the antibiotic resistance profile of the pathogen, detailed in the image as which genes the pathogen expresses.
The system then references these genes against a database of available antibiotics, and suggests which are the most suitable. Again, using the image as an example, the higher the number the lower the chances of the antibiotic being able to treat the disease, so here the physician knows instantly that Cefepime is unlikely to be effective, but Tigecycline should almost certainly solve the issue. This process can take days as things stand, and many patients can die during that period, which is the reason for the current inefficient and potentially dangerous cocktail approach. With this system in place, lives can be saved, and costs cut.
Where are we from a time frame standpoint? Lighthouse is ready and commercially available right now, and is filling up with data. The company aims to have the above process (albeit perhaps taking 2 or 3 hours) active globally by mid 2017. By late 2018, it OpGen expects the one-hour test to be established.
The takeaway here is that Merck and OpGen are working to not just improve the antibiotic resistance landscape, but make it unrecognizable from its current position. Merck is the biggest company in the world from an antibiotic standpoint, and it’s very much in the company’s interests for the healthcare sector to not only be able to accurately diagnose infectious diseases, but also to treat them as effectively as possible. This extends the lifespan of its portfolio of products. More accurate diagnosis leads to fewer resistance buildups. The OpGen test and technology platform directly complements this interest, and Merck’s 37.5% stake in the former underlines this complementing quantifiably.




